How Can You Use Clinical Significance to Support Positive Outcomes in Your Project?
Abstract
The fecal occult blood test (FOBT) is a screening tool for hematochezia. This study aims to summarize the clinical features associated with a positive FOBT in neonates and to explore some clues for the underlying causes. Combination with other clinical information, identifying the possible etiology is more likely and could be useful for choosing an effective therapeutic strategy. The medical records of 282 neonates with positive FOBTs from January ane to July 31, 2016, were collected and retrospectively analyzed. The total incidence rate of FOBT positivity in neonates was half-dozen.2%. Among these patients, 71 (25.two%) neonates had false-positive FOBTs, whereas 211 (74.8%) neonates had intraintestinal sources of hematochezia. Necrotizing enterocolitis (NEC, xx.9%), structural abnormalities of gastrointestinal tract (SAGT, 12.4%), and suspected food allergy (sFA, x.half-dozen%) were the most common causes of neonatal hematochezia. It indicated that FOBT-positive neonates with NEC were more likely to suffer due to a younger gestational age, lower birth weight, and lower weight on admission than the neonates with other conditions. The proportions of neonates with bloody stool (90.0%) and diarrhea (63.3%) in the sFA grouping were markedly college than those in the other groups. All the same, in the SAGT group, emesis (94.3%) and abdominal distension (lxxx.0%) were patently college, usually accompanied by a relatively poor response (threescore.0%) and weakened bowel sounds (48.half-dozen%). Furthermore, the college incidences of poor response (72.i%), abdominal amplification (71.2%), bloody stools (64.4%), and weakened bowel sounds (62.7%) were observed in the NEC grouping. Due to the complicated etiology associated with a positive FOBT, the analyzed indexes were combined with other clinical features to identify the likely causes of neonatal hematochezia. Because NEC, sFA and SAGT show similar clinical manifestations and can occasionally transform into each other, close and frequent observation is crucial for timely intervention to attain a better prognosis. Although it failed to provide an early on alarm of severe disease through FOBT, and the early intervention for FOBT might not decrease NEC, sFA, structural bowel injuries, or any other complications, newborn FOBT positive reminds medical staff to be alert to the related diseases including NEC, SAGT and sFA, by closer ascertainment and follow-up.
Introduction
Hematochezia, a common phenomenon amidst neonates, is defined as gastrointestinal bleeding due to a diversity of causes involving digestive tract disorders and comorbidities of some critical illnesses, such as necrotizing enterocolitis (NEC), intestinal malrotation and volvulus, Hirschsprung affliction, infectious colitis and systemic coagulopathy1,2.
The fecal occult claret examination (FOBT), a screening examination for hematochezia, is employed to observe invisible or subconscious (occult) blood in the feces. It is simple and noninvasive. In adults, the FOBT is used as a screening tool for colorectal cancer associated with intestinal mucosal injuryiii. Even so, etiological data associated with positive FOBTs in neonates is scarce due to the particularity of the newborn population. It was reported that the positivity rate of FOBT in neonates is approximately 8.5%iv, but it could be college in extremely depression birth weight neonates. Abramo et al. reported that the incidence rate of occult blood was 10% among neonates that were <1,800 g at nativity5.
This study aimed to retrospectively clarify the characteristics associated with positive FOBTs in neonates admitted to our neonatal intensive care unit (NICU) by comparing the clinical characteristics and final diagnoses and attempting to explore some clues for improving efficiency of diagnosis and treatment.
Results
Underlying causes of positive FOBTs in neonates
Among the 282 neonates with positive FOBTs, 71 neonates (25.two%) had false-positive results, while the remaining 211 neonates (74.8%) had intraintestinal sources of bleeding. NEC, structural abnormalities of the gastrointestinal tract (SAGT) and suspected food allergy (sFA) were the well-nigh common causes of neonatal hematochezia and occurred in 59 neonates (xx.ix%), 35 neonates (12.four%), and 30 neonates (x.six%), respectively. Other etiologies included acute stress ulceration in 29 neonates (x.three%), acute diarrhea in 27 neonates (nine.6%), postsurgical intestinal bleeding in 12 neonates (4.3%), functional abdominal distension in 10 neonates (3.five%), feeding intolerance in eight neonates (ii.viii%), and meconium constipation in i neonate (0.four%). False-positive FOBT results were caused by fecal contamination (often caused by pseudomenstruation and hematuresis) or other extraintestinal sources, including swallowed maternal claret (ingested during commitment or from split nipples) and neonatal blood (catheter-induced trauma to the upper airway or gastric mucosa).
Clinical characteristics of neonates with NEC, SAGT and sFA
The clinical data for the first three etiologies in FOBT-positive neonates was analyzed. Showtime, focus was directed to the onset fourth dimension of the positive FOBT, and it was found that the median (IQR) onset times for NEC (7 [3, 13] days, data are presented equally Median [P25, P75]), SAGT (10 [4, 17] days), and sFA (13 [eight.75, xx.25] days) were significantly dissimilar (Ten ii = 9.318, P = 0.009). The gestational age (GA) (258 ± twenty) days and nascence weight (BW) (2.seventy ± 0.64) kg in the SAGT group were significantly lower than those in the NEC group (272 ± 13) days and (3.17 ± 0.54) kg respectively, whereas in the sFA group (270 ± 12) days and (iii.19 ± 0.42) kg, respectively (P < 0.001). In add-on, the weight on access in the NEC group (2.60 ± 0.64) kg was plain lower than those in the SAGT and sFA groups (three.00 ± 0.53) kg and (three.xiii ± 0.45) kg, respectively (P < 0.001, Tabular array i). The other observed items included gender, eutocia, gravity and parity, which did not have statistical differences (P > 0.05). These data indicated that neonates with NEC with positive FOBTs were more likely to suffer from a younger GA, lower BW, and lower weight on admission than those with other conditions.
Risk factors and accompanying symptoms of neonates with NEC, SAGT and sFA
The differences in the delayed excretion of meconium, feeding patterns and the utilization of antibiotics among the three groups were statistically pregnant in terms of adventure factors (P < 0.01). The proportion of neonates with delayed excretion of the meconium in the SAGT group was 37.1%, which was significantly higher than those in the other ii groups (P < 0.01).The proportion of formula feeding and the administration of antibiotics earlier a positive FOBT in the NEC group was 61.0% and 52.5%, respectively, which were significantly higher than those in the other two groups (P < 0.01). The rates of accompanying symptoms, emesis, abdominal distension, diarrhea, encarmine stool, weakened bowel sounds and poor response were all statistically pregnant among the 3 groups (P < 0.05). Furthermore, the proportions of neonates with bloody stool (ninety.0%) and diarrhea (63.three%) in the sFA group were markedly higher than those in the other groups. The rates of emesis (94.iii%) and intestinal distension (80.0%) were plainly higher in the SAGT group than in the other groups, and these symptoms were accompanied by a relatively poor response (lx.0%) and weakened bowel sounds (48.half-dozen%). Furthermore, high incidence rates of weakened bowel sounds (62.7%), poor response (72.1%), intestinal amplification (71.2%), and bloody stool (64.four%) were observed in the NEC group (Table 2).
Auxiliary examinations of the neonates with positive FOBTs due to NEC, SAGT and sFA
Consummate claret count (CBC) indicated that the percentage of neutrophils was significantly increased in the NEC (55.4%) and SAGT (57.i%) groups (P < 0.001). Furthermore, the pct of eosinophils in the NEC (7.6%) and sFA (vii.viii%) groups was obviously college than those in SAGT grouping (4.1%) (P < 0.05). The platelet count in the sFA group was significantly elevated, reaching an average of 393 × 109/L (P < 0.05), whereas the counts in the other two groups were 316 × 109/L and 311 × 10nine/50, respectively. The FOBTs in sFA neonates often showed elevated eosinophils and/or platelets in the CBC, which usually indicates vasculitis related to an allergic reaction, while the neonates in the NEC and SAGT groups often showed increased levels of neutrophils. Abdominal radiography revealed that the neonates in the NEC group mainly had a severe degree of bleeding (47.iv%), whereas those in the sFA group (48.1%, moderate degree) appeared to have a slightly more severe degree than those in the SAGT group (44.one%, balmy degree) (Tables two and iii).
Prognosis of the neonates with positive FOBTs due to NEC, SAGT and sFA
The prognoses included improvement and withdrawal from therapy. Improvement was defined every bit a marked alleviation. The neonates that showed improvement were farther classified into the medical handling grouping or the surgical & medical treatment group. In contrast, withdrawal from therapy was defined as discharged from the hospital too early considering of serious complications or economical limitation.
It is clear that comeback was the primary outcome in all three groups, bookkeeping for more than than lx.0% of the total. A total of 86.7% of sFA neonates, 57.6% of NEC neonates and 14.3% of SAGT neonates received medical treatment, whereas 68.vi% of SAGT neonates and 6.eight% of NEC neonates underwent surgical treatment. Moreover, 35.5% of NEC neonates, 17.1% of SAGT neonates, and thirteen.3% of sFA neonates were withdrawn from therapy. The differences among these groups were statistically meaning (Ten 2 = 6.861, P = 0.032; Table two). In the NEC group, 21 neonates were withdrawn from therapy due to serious complications, including homeostasis disturbances, mail-NEC intestinal stricture, and short bowel syndrome. Withal, 4 patients in the sFA group were discharged before complete enteral feeding due to economical factors or emotional factors such as unbearable being separated from their babies.
Values of the clinical characteristics in the diagnosis differentiation of NEC, SAGT and sFA
To determine whether the statistically significant indexes in Table 2 were valuable for the differential diagnosis, the indexes were subjected to a multivariate assay, including a discriminant assay and multiple logistic regression analysis (Tables two and four). The discriminant assay indicated a correlation of BW (10ane), delayed excretion of the meconium (Xii), emesis (Xthree), diarrhea (104), bloody stools (Xv) and poor response (X6) with NEC (YNEC = 0.010Xi + ane.515Xii + 3.641X3 − ane.201X4 + four.029X5 + half-dozen.761X6 − 19.433), SAGT (YSAGT = 0.012Xi + 4.291X2 + vi.002Xiii − ane.619X4 + two.644Xv + six.595X6 − 25.853), and sFA (YsFA = 0.011X1 + 2.410X2 + 3.472X3 + 0.491X4 + 5.182X5 + 4.686Xsix − 22.395). The maximum Y value was chosen, and the predicted probability was 71.0%, whereas the multivariate logistic regression analysis revealed a correlation of onset time (101), antibody application, emesis (10ii), and diarrhea (X3) with NEC (YNEC = −2.634 − 0.105X1 − 1.862Xtwo + 2.091X3) and SAGT (YSAGT = −10.654 − 0.125Xi − 2.59X2 + two.651Xthree) when because the sFA group as a reference. The maximum probability was chosen, and the predicted probability was 77.4%. The difference in the overall predicted probability between the 2 models was not statistically meaning (Ten two = 1.348, P = 0.246; Table 4).
Discussion
Hematochezia is common during the neonatal period, manifesting as visible bloody stool or positive FOBT. The etiology is complicated, including the diseases of digestive tract and/or the complications of many critical disorders. Early identification of the cause is the key to its successful management. Due to the small amount of blood, some patients practice not present visible blood in the stool, and a FOBT is needed to reduce misdiagnoses. Therefore, this report retrospectively analyzed the clinical characteristics of FOBT-positive neonates, providing a clinical feel for the etiological diagnoses and appropriate effective treatments. Our section was the largest NICU in western Communist china. A total of 5,330 neonates were admitted from January 1 to July 31, 2016, including 1183 premature neonates and 4147 full-terms. Most of them suffered from perinatal asphyxia, severe pneumonia, sepsis, severe hemolysis and jaundice at or beyond the threshold level for commutation transfusion, prematurity and other critical illnesses. As a tertiary hospital affiliated of the medical university and the middle of neonatal emergency-transportation organization in western China, many neonates admitted to our section are transferred from out-of-town areas and are separated from their family, resulting in a relatively low charge per unit of breastfeeding, approximately 30%, which is also a chance gene for intestinal impairment, reflected as FOBT positivity. Therefore, the FOBT is employed as a routine screening test in our NICU. A number of weather are related with positive FOBTs among neonates. Systemic issues related to hemorrhagic diseases or coagulopathy cause positive FOBTs. However, none of these disorders were institute in this written report, indicating that the incidence rate of occult hematochezia caused past systemic disorders in neonates is non as loftier as previously reported (1–two%)6. The present data revealed that the full incidence rate of FOBT positivity was 6.two%, and interestingly, 25.ii% (71/282) of positive FOBTs in neonates were false-positives, which were caused by contaminated carrion or the swallowing of maternal or neonatal blood. Furthermore, 74.8% (211/282) of bleeding was due to abdominal sources of hematochezia. Among these, NEC, SAGT and sFA were the well-nigh common causes, comprising 20.9%, 12.iv% and 10.6% of the total positive FOBTs, respectively.
The onset time of NEC was inversely correlated with GA. NEC tin can present within the first calendar week of life in term infants, whereas in preterm infants, it usually appears after commencement of feeds and occurs afterward the iind and threerd weeks of lifeseven. In this written report, the average onset time of NEC in FOBT-positive infants was on the 7th day after nascency, which was probably related to preterm commitment in 35weeks of the 59 neonates with NEC. Furthermore, it was indicated that a neonate with a young GA, depression rate of breastfeeding, exposure to antibiotics, and symptoms such as abdominal distention, weakened bowel sounds, or poor response should exist considered to occurrence of NEC. In this situation, a CBC and intestinal radiography must exist immediately carried out. Indeed, hematological abnormalities commonly convey certain important and valuable prognostic information. Maheshwari et al.8 noted that increased neutrophil counts comprise an appropriate inflammatory response in patients with mild-moderately severe disease. In dissimilarity, neutropenia tin exist seen in astringent NEC. The nowadays data showed that neonates in the NEC group had elevated neutrophil counts, which may be related with 64.iv% [38/59] neonates in the NEC group diagnosed as stage I NEC. Additionally, Yang Y et al.ix reported that, neutrophil/lymphocyte (N/50) ratio could exist good mark for the early on diagnosis of NEC, distinguishing the severity. The data showed that neonates in the NEC group had elevated (North/L) ratio. Due to the small sample of NEC neonates, sub-group analysis was not performed, and the data was too express to distinguish the severity. Big sample, multi-center studies are needed.
Traditionally, intestinal radiography has also played a crucial role in the diagnosis of NEC. Neonates with NEC ofttimes have severe intestinal lesions, which mainly reveal focal distention, fixed bowel loops, pneumatosis and portal venous gas on abdominal radiography. Furthermore, some of the neonates with NEC in this written report presented with typical signs, categorized every bit moderate and severe intestinal injuries, on abdominal radiography (Tables 2 and 3). Wang et al.x revealed that the recovery rate of NEC was lxx–80%, whereas the improvement charge per unit of NEC was 64.4% (38/59) in this study. Amidst the studied neonates, 34 received conservative treatment, iv underwent surgery due to perforation or complete obstacle, and 21 were withdrawn from therapy due to serious complications, including homeostasis disturbances, post-NEC intestinal strictures, and brusk bowel syndrome. Gaudin et al.11 investigated the risk factors related to post-NEC intestinal stricture and indicated that the presence of peritonitis signs and thrombopenia were risk factors. Zhang et al.12 indicated that a tardily-onset time was a predictor of post-NEC intestinal stricture and that the summit of white blood cells (WBCs) and procalcitonin (PCT) were observed in neonates with post-NEC abdominal stricture.
Previous studies have suggested that the incidence of sFA obviously increases subsequently NEC or alimentary canal surgery13,14. The symptoms of sFA are diverse and mainly occur from the 2nd to ivth week afterward contact with a food protein or other suspected substances. It was constitute that the onset time of a positive FOBT caused by sFA mostly appeared on the 2nd week of life, and 93.3% (28/xxx) of the infants with GA more 35 weeks. In addition, the incidence rates of gross bloody stools and diarrhea were xc.0% and 63.3%, respectively. Elevated eosinophil and platelet counts in the CBC appeared to bespeak an allergic disorder, which was consequent with Feuille's findingsxv. The signs on abdominal radiography mainly show diffuse distention and the separation or focal thickening of bowel loops. However, Kawai Thou et al.16 reported that the signs on abdominal radiography in infants with sFA presented recurrent episodes of pneumatosis-like NEC, which was difficult to differentiate from NEC. Similar radiographic signs were found in half dozen neonates in this study. In terms of treatment, 86.7% (26/30) of the neonates improved after food avoidance, as observed in the nowadays study. Suda et al.17 reported that some cases of sFA later on adult into NEC. They suggested that a persistent decrease in the platelet count may betoken this trend. Therefore, dynamic follow-upward of CBC should be performed to monitor progress timely.
Based on the present statistical data, it was establish that Hirschsprung illness, intestinal stricture and intestinal atresia were frequent malformations in FOBT-positive neonates in the SAGT grouping, and the proportions were 37.1% (13/35), 14.iii% (5/35), and 14.3% (5/35), respectively. Gosain et al.18 reported that neonates with Hirschsprung disease were at high take chances for Hirschsprung-associated enterocolitis. The present data concord with this, as 13 neonates with positive FOBTs who had NEC-similar clinical characteristics were finally confirmed to suffer from SAGT. Amidst these neonates, eight had Hirschsprung disease, four had abdominal stricture, and i had intestinal atresia. Of the SAGT neonates with positive FOBTs, 37.one% (13/35) had delayed excretion of the meconium, whereas 94.3% (33/35) had emesis. The CBC revealed elevated neutrophil counts, indicating the possibility of secondary infection. Since enteral structural abnormalities vary, unlike intestinal imaging characteristics contribute to diagnosis differentiation. Surgery can provide a definitive diagnosis but may not be suitable for repairing the intestinal structural abnormalities. Given this invasive approach, which may lead to postoperative complications such as agglutinative abdominal obstruction, NEC and allergic enteritis, a precise grasp of the surgical opportunity is vital. In the present study, 68.6% (24/35) of the neonates with enteral structural abnormalities and positive FOBTs underwent surgery. Amid these neonates, 5 neonates were readmitted for complications, three neonates had adhesive intestinal obstructions and two presented NEC within one year after the operation. Follow-up examinations were conducted on the readmitted patients. Yet, the information were still limited in reflecting the actual long-term prognosis.
SAGT occurs in neonatal menstruation, including built and caused. Congenital SAGT tin can be considered as malformations of gastro-intestinal tract. NEC, sFA and SAGT take the similar clinical manifestations, which sometimes transform into each other (Fig. 1). Built and acquired SAGT may cause intestinal obstruction and, consequently, local infection or inflammation due to impairment to the intestinal bulwark, resulting in a hypersensitivity to certain specific dietary antigens, manifesting as food allergy. If physicians encounter infants with surgical gastrointestinal affliction, including intestinal malrotation, they need to consider food allergy in the differential diagnosis or as a complicating gene13. Stricture after NEC is a well-known common complication. Later on the acute episode of NEC, stricture, which is associated with astringent and prolonged morbidity (septicemia, perforation, intestinal obstruction) and morbidity secondary to intestinal stricture, can develop during a variable period irrespective of the fashion of management. Food allergy is a hypersensitive reaction to sure specific dietary antigens. Suda et al.17 reported that two neonates with sFA required laparotomy due to secondary NEC. Intestinal edema and injury would be induced when proper abstention of suspected-food is not practiced, and severe abdominal inflammation might progress to local necrosis and perforation or endogenous infection, mimicking NEC and causing enteral complications such as intestinal stricture and other acquired SAGT. Even so, the treatments and prognoses of NEC, sFA and SAGT are commonly different. Therefore, the investigators attempted to plant predictive models by discriminant analysis and multiple logistic regression analysis. Emesis and diarrhea are both involved as indexes in the two models, suggesting that these may accept some clinical significance in the diagnosis. Unfortunately, no statistically meaning difference was found in the overall predictive charge per unit of these two models. Thus, no effective approach can be provided for the differential diagnosis at present. Hence, a prospective study is recommended to establish a valuable clinical prediction model.
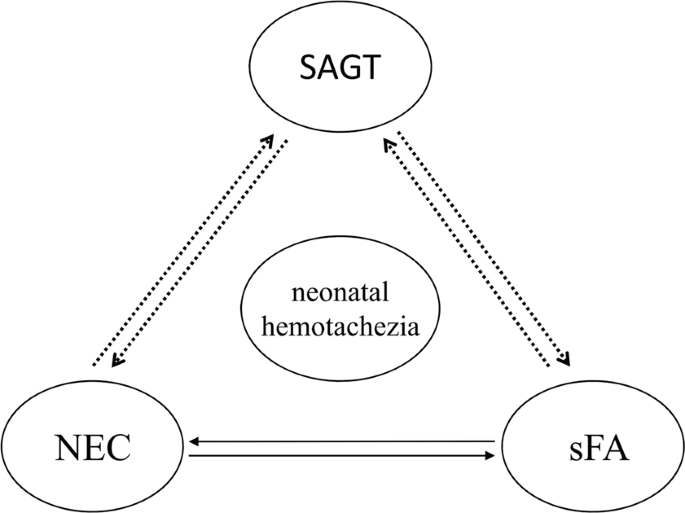
Common etiology of neonatal hematochezia.
In summary, for neonates with positive FOBTs, simulated-positive results should showtime be excluded. Then, systemic diseases and digestive tract disorders, such as infection, deformity, allergy, stress and injury, should be identified1,nineteen co-ordinate to the process described in Fig. two. NEC, SAGT and sFA were the nigh common causes of neonatal hematochezia. In newborns, those diseases testify the like clinical manifestations, and can occasionally transform into each other under some weather condition. Pickering A et al.20 have reported that routine fecal occult blood testing does not predict necrotizing enterocolitis. Therefore, although we could not provide an early warning of severe illness though FOBT, and the early intervention for FOBT might not decrease NEC, sFA, structural bowel injuries, or any other complications, the significance of newborn FOBT positivity lies in that, medical staff would exist alarm to the related diseases including NEC, gastrointestinal malformations and suspected food allergy, with closer observation and follow-up. Based on the combination of the full general condition, feeding tolerance, temperature, abdominal signs, CBC, routine stool tests plus FOBTs, and abdominal image examinations, clinicians would be able to identify the possible etiology, which is useful for timely modulating in the therapeutic strategy.
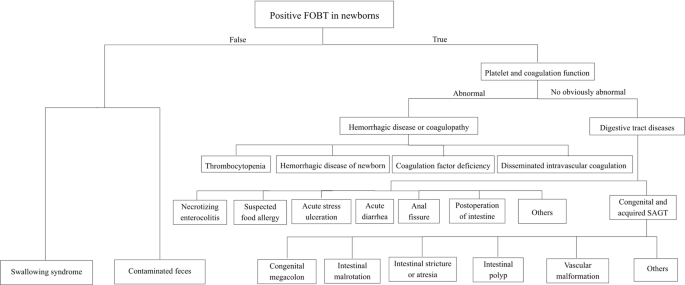
The diagnostic flow chart of positive FOBT in neonates.
Methods
Study setting and patient selection
This written report was conducted in the Neonatology Department of the Children's Infirmary of Chongqing Medical University. The information were collected from medical records of the Neonatology Section from January 1 to July 31, 2016. The study was approved by the Institutional Review Lath of the Children's Infirmary of Chongqing Medical Academy. All methods were performed in accordance with the relevant guidelines and regulations. The information were nerveless, reviewed, deidentified, and analyzed anonymously by the authors; the ethics commission waived the requirement for informed consent because of the anonymized nature of the data and scientific purpose of the report.
Subjects
A total of 5,330 neonates were screened. Amongst them, 1183 neonates were premature including 140 very low birthweight newborns. 330 neonates with positive FOBTs were preliminarily registered in the nowadays study. The incidence charge per unit of FOBT positivity was 6.2%. Two neonates with the incomplete medical records, and 46 neonates who had hematochezia after 28 days or whose GA ≥ 42weeks, were excluded. Thus, a total of 282 neonates were finally enrolled. The stool of individuals was tested at least once, 60 neonates were tested once and the others were tested twice or more. Among these subjects, 90 had a history of grossly visible bloody stools, and the FOBT was performed after the gross encarmine stools disappeared.
Information drove
Demographic, commitment and feeding history, concrete examination (accompanying symptoms), treatment tape, CBC and other specific examinations, including abdominal plain movie test (the well-nigh astringent result was considered if in that location were multiple re-examinations), all data were collected from the Electronic Medical Tape (EMR). NEC was divers based on Bell's criteria with modifications21.
Adverse reactions associated with FA are frequent in the first year of life22. A challenge test with the causal food is indispensable in the diagnosis of food allergy but is not realistic for all cases in newborns23, considering these tests may be dangerous and the results were difficult to clarify in neonates. Therefore, the concept of suspected food allergy might be more suitable for these cases. In our study, the diagnosis of sFA was based on a combination of some of the followings, a family history of anaphylactic diseases, a history of direct or indirect exposure to antibiotics and/or other suspected substances, and the exclusion of other possible causes of bloody stool. In addition, the symptoms were relieved with the feeding of amino acid milk powder or suspected-food avoidance, relapsing afterward the ingestion of the suspected nutrient.
Acute stress ulcer is diagnosed co-ordinate to preterm and term infants in the neonatal intensive care unit develop gastric mucosal lesions and present with upper GI bleeding suggested by gastric lavage fluid and have the exposure stress factors which includes perinatal asphyxia, intracranial hemorrhage, increased intracranial pressure level, sepsis, hypoglycemia, severe vomiting, etc24.
Acute diarrhea was diagnosed according to the increased frequency and/or the changed characteristics of the stool compared to normal stool, whereas newborn diarrhea features the passage of loose or watery stools at least vi times within 24 hours.
Structural abnormalities of the alimentary canal (SAGT) were diagnosed based on biopsy or respective postoperative results, means "congenital or caused SAGT".
Fecal occult blood examination
FOBTs were performed at our clinical laboratory using the colloidal gold method (Aibo occult claret detection reagent; Aibo Biomedical, Hangzhou, China). Briefly, a stool sample was nerveless from the diaper. Then, a minor amount of the collected fecal specimen was smeared in a test tube and immediately taken to the clinical laboratory. The assay was performed according to the product instructions. The outcome was considered positive when both the detection line and the quality control line appeared.
Evaluation of intestinal radiography
Abdominal radiography was evaluated based on the Duke Abdominal Assessment Scale (DAAS)25. Since reduced intestinal inflammation is not included in the DAAS, this was analyzed separately. The degree of severity referred to the study by Boyin Deng et al.26 (Table 3).
Statistical assay
All data were analyzed using SPSS 17.0 software (Chicago, IL, USA). Normally distributed continuous data were described as the mean ± standard divergence (1000 ± SD) and examined by analysis of variance. Skewed data were described equally the median (interquartile range [IQR]) and analyzed past the Kruskal-Wallis exam. Categorical data were analyzed by the chi-square test or Fisher's exact exam. A multivariate analysis, including discriminant and multiple logistic regression analyses, was practical to analyze the differential diagnosis. A P-value < 0.05 was considered statistically significant.
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of the Children's Infirmary of Chongqing Medical University.
Informed consent statement
This is a retrospective report. The ethics commission waived the requirement for informed consent because of the anonymized nature of the data and scientific purpose of the report.
References
-
Romano, C. et al. Pediatric gastrointestinal bleeding: Perspectives from the Italian Social club of Pediatric Gastroenterology. World J Gastroenterol 23, 1328–1337 (2017).
-
O'Neil, A. M. & Homme, J. L. Evaluation of Hematochezia in a Two-Day-Old Infant. J Emerg Med l, 41–43 (2016).
-
Commission, O. H. T. A. Fecal occult blood test for colorectal cancer screening: an evidence-based analysis. Ont Health Technol Assess Ser 9, 1–40 (2009).
-
Noland, J. L., Stahl, G. E. & Anday, Eastward. One thousand. Event of maternal cocaine on neonatal gastrointestinal tract. Pediatr Res 29, 101 (1991).
-
Abramo, T. J., Evans, J. S., Kokomoor, F. W. & Kantak, A. D. Occult blood in stools and necrotizing enterocolitis. Is at that place a relationship. Am J Dis Child 142, 451–452 (1988).
-
Buchanan, M. R. Coagulation disorders in the neonate. Pediatr Clin North Am 33, 203–220 (1986).
-
Yee, W. H. et al. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics 129, e298–304 (2012).
-
Maheshwari, A. Immunologic and Hematological Abnormalities in Necrotizing Enterocolitis. Clin Perinatol 42, 567–585 (2015).
-
Yang, Y. et al. Does neutrophil/lymphocyte ratio have expert diagnostic value in neonatal necrotizing colitis. J Matern Fetal Neonatal Med 32, 3026–3033 (2019).
-
Wang, Ten. L., Shao, 50. P. & Xie, W. Y. Analyses of 164 cases neonatal necrotizlng enterocolitis. Chinese Journal of Pediatric Surgery 36, 105–108 (in Chinese) (2015).
-
Gaudin, A. et al. Necrotizing enterocolitis (NEC) and the gamble of abdominal stricture: the value of C-reactive protein. PLoS One 8, e76858 (2013).
-
Zhang, H. et al. Predictive factors and clinical practice profile for strictures post-necrotising enterocolitis. Medicine (Baltimore) 96, e6273 (2017).
-
Matsuki, T. et al. Intestinal malrotation with suspected cow's milk allergy: a case report. BMC Res Notes 5, 481 (2012).
-
Wei M. L. Westward. B. & Chen, P. J. A case study on neonatal allergic colitis with similar symptom to NEC and literature review. Chinese journal of child health 25, 1277–1280 (in Chinese) (2017).
-
Feuille, East. & Nowak-Węgrzyn, A. Definition, etiology, and diagnosis of nutrient protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 14, 222–228 (2014).
-
Kawai, M. et al. Cow's milk allergy presenting Hirschsprung'due south affliction-mimicking symptoms. Pediatr Surg Int 21, 850–852 (2005).
-
Suda, K. et al. Aggressive gastrointestinal nutrient allergy in neonates and its possible human relationship to necrotizing enterocolitis. Int J Surg Case Rep 36, 175–178 (2017).
-
Gosain, A. et al. Guidelines for the diagnosis and management of Hirschsprung-associated enterocolitis. Pediatr Surg Int 33, 517–521 (2017).
-
Bray-Aschenbrenner, A., Feldenberg, L. R., Kirby, A., Fitzpatrick, C. Thousand. & Josephsen, J. B. Bloody Stools in a 3-Day-Old Term Baby. Pediatrics 140 (2017).
-
Pickering, A., White, R. & Davis, N. L. Routine fecal occult blood testing does not predict necrotizing enterocolitis in very low birth weight neonates. J Neonatal Perinatal Med nine, 171–178 (2016).
-
Walsh, M. C. & Kliegman, R. M. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin Northward Am 33, 179–201 (1986).
-
Kvenshagen, B., Halvorsen, R. & Jacobsen, M. Adverse reactions to milk in infants. Acta Paediatr 97, 196–200 (2008).
-
Miyazawa, T., Itahashi, K. & Imai, T. Direction of neonatal cow'south milk allergy in high-take chances neonates. Pediatr Int 51, 544–547 (2009).
-
Shao, 10., Ye, H. & Qiu, X. Applied Neonatology (4th Edition). People's Medical Publishing House, p.477–482. (in Chinese ) (2011).
-
Coursey, C. A. et al. Radiologists' agreement when using a 10-point scale to report intestinal radiographic findings of necrotizing enterocolitis in neonates and infants. AJR Am J Roentgenol 191, 190–197 (2008).
-
Deng, B. Y. HE, H. Y. & Yu, Grand. R. The Study of Radiographic Duke Abdominal Assessment Calibration in Neonatal Necrotizing Enterocolitis. Periodical of Clinical Radilolgy 33, 912–915 (2014).
Acknowledgements
This study was supported by grants from the Clinical Research Project of Children's Hospital of Chongqing Medical Academy (YBXM 2019-007). Nosotros thank professor Yan Hu, Pediatrician and allergist of Children's Hospital of Chongqing Medical University, for the consultation virtually food allergy. We give thanks Dr. Dapeng Chen, the director of clinical laboratory center of Children's Hospital of Chongqing Medical University, for the technical consultation nigh fetal occult blood exam. We capeesh greatly Mr. Wanchun Wu, the managing director of information center of Children'southward Infirmary of Chongqing Medical University, for the technical help in collection of the medical records. The authors are grateful to the reviewers for their valuable comments and suggestions, which improved the paper.
Author information
Affiliations
Contributions
All authors helped to perform the enquiry; Qiuping Wen and Kaizhen Liu manuscript writing, performing procedures and information analysis, they contributed every bit to this report, should be regarded every bit first articulation authors. Weihong Yue performing experiments and information analysis; Shiqi Shao contribution to writing the manuscript; Shu Zhang assistant in data drove and analysis; Xiaoqing Li contribution to drafting conception and design; Ziyu Hua contribution to writing the manuscript, drafting conception and blueprint. All authors participated in manuscript edits and approved the final version.
Respective writer
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This commodity is licensed under a Artistic Commons Attribution four.0 International License, which permits utilize, sharing, adaptation, distribution and reproduction in any medium or format, every bit long as you give appropriate credit to the original writer(southward) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third political party material in this article are included in the article'southward Creative Commons license, unless indicated otherwise in a credit line to the cloth. If fabric is non included in the article's Creative Commons license and your intended use is non permitted by statutory regulation or exceeds the permitted employ, you will demand to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/past/4.0/.
Reprints and Permissions
About this article
Cite this commodity
Wen, Q., Liu, K., Yue, W. et al. Clinical significance of positive fecal occult blood test in neonates. Sci Rep 9, 17898 (2019). https://doi.org/10.1038/s41598-019-54511-5
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1038/s41598-019-54511-5
Comments
By submitting a comment you concord to bide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Source: https://www.nature.com/articles/s41598-019-54511-5
0 Response to "How Can You Use Clinical Significance to Support Positive Outcomes in Your Project?"
Post a Comment